It feels strange to blog about ideal diets when my day-to-day work is so far removed from the advice I’ve been giving on these blogs. As things are expected to get really busy this week, I thought I would just take this opportunity to let you know a little bit more about what Dietitians like myself are doing right now during the COVID-19 crisis.
Feeding those with COVID-19
As a Nutrition Support Dietitian on the Surgical, Gastroenterology and Critical Care wards, I have always been involved in helping people who are unable to eat normally. We are all now aware that many patients with COVID-19 will require ventilators.
If you are ventilated, you are NOT able to eat.
COVID-19 patients may commonly stay on a ventilator for two weeks. If they were to receive no nutrition at all during this time, they would become extremely weak and their chance of recovery would be greatly reduced.
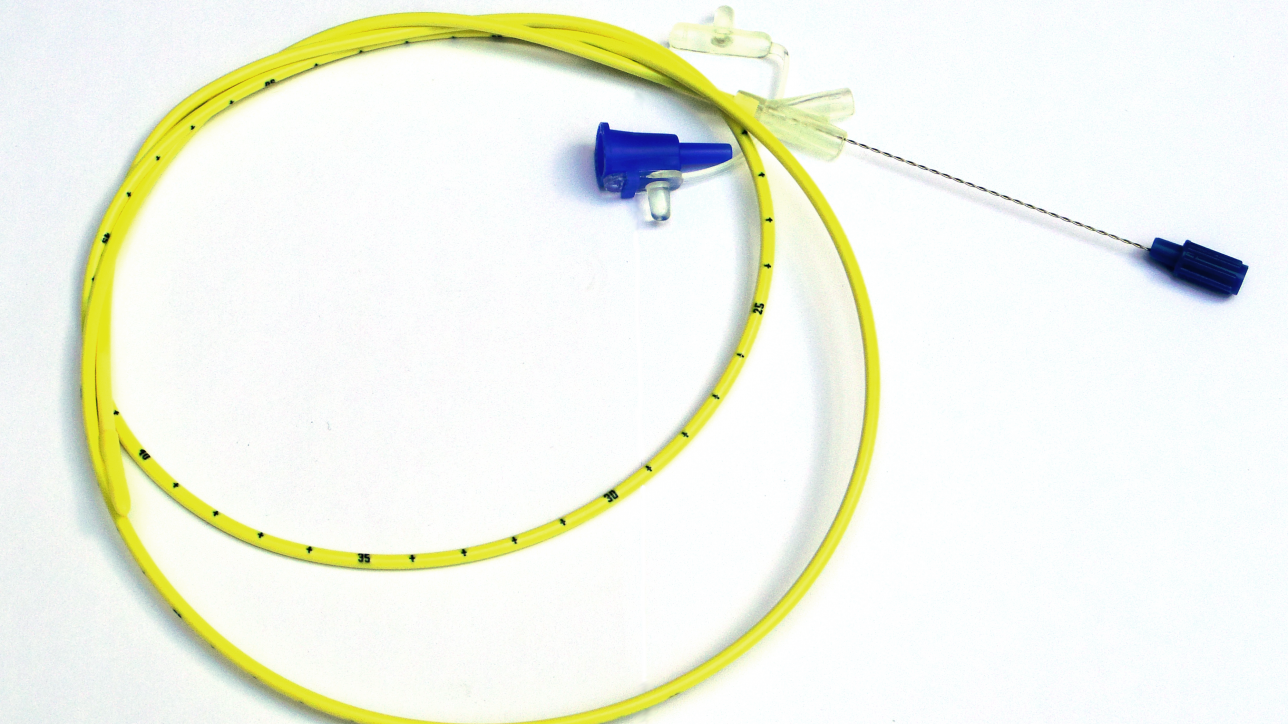
Most of these patients are therefore fed through a nasogastric tube via a pump. Each patient should have the feed tailored to their individual needs by the Critical Care Dietitian as overfeeding will put additional strain on their respiratory system whereas underfeeding will obviously mean they miss out on the full benefits. The amount of feed each patient requires varies according to a number of factors including their age, weight, gender and other drugs and infusions they may be receiving at the time, meaning that I would normally review them on an almost daily basis.
Dealing with complications
Many of these patients also experience a failure of their digestive system due to their immobility and all the medications they are on – meaning that I then need to alter the feed rate, type of feed or advise on alternative ways of feeding. Should a patient require intravenous feeding, for example, then I would review them daily to advise on the levels of fat, glucose, protein, sodium, potassium, magnesium, calcium and phosphate that should be added to the feed – depending on their blood results that day.
Dealing with the increase in patients
As the number of patients on critical care has rapidly increased, we have had to think about alternative ways of working.
Those of us who regularly work on the wards have been busy up-skilling our colleagues who normally work in less acute areas and have kindly come into the hospitals to join us.
We have put a lot of work in to designing “off the peg” feed regimens that will still be safe to use with certain groups of patients. We have been working hard to ensure that enough feed pumps are available – and putting alternative plans in place should we run out. There are methods of tube-feeding that can be used without pumps but these are labour-intensive and it is unlikely that hard-pressed nurses will have time; myself and my colleagues are likely to have to become much more “hands-on” over the next few months as we support our Nursing colleagues – especially those who have themselves been drafted in from other areas and are new to this level of care.
Regular patients still need care
Outside of Intensive therapy units (ITU), we have seen other patient groups moved to our rehabilitation hospitals and we have had to provide emergency training to our Dietetic colleagues there, who would not normally see that patient group. We still need to try to provide the same level of care to patients coming into hospital with strokes, heart attacks, cancers and all the usual problems; and as well as that we are trying to identify and help those patients with conditions such as inflammatory bowel disease, diabetes, coeliac disease and disease-related weight-loss who have had their outpatient appointment cancelled.
I hope that this helps to raise the awareness of the role of the Dietitian within a hospital, and the value of the profession at this time. I will still be available to help people who are struggling with their own issues at this difficult time – particularly gut issues such as IBS, which tend to become worse with stress. I am able to provide consultations via Skype, Zoom, WhatsApp or telephone – however please bear with me if time-slots are more limited that usual just at present!
More information about nutrition and COVID-19 can be found on the British Dietetic Association website.